
The field of immunotherapy is constantly evolving with the ultimate goal to develop new treatments that help the body’s immune system fight cancer. Immune cells, such as T cells and natural killer (NK) cells, have the inherent ability to combat diseases, including cancer, but are often inhibited by the body’s own suppressive mechanisms. Cancer immunotherapies such as checkpoint inhibitors (CPIs) were designed to counteract these. Today, there are many approved immunotherapy approaches that can enhance the anti-tumour activity of immune cells, resulting in improved survival rates. However, even as science advances, there remain patients who still need new treatment options. By re-engineering existing approaches that have already shown clinical promise, there is potential to bring further benefit to the patient community in its fight against cancer.
Unlocking the potential of immunotherapies
Decades ago, antibodies targeting the protein CD20, found on B cells, revolutionised the way we treat some leukaemias and lymphomas. Since then, several next-generation antibodies have been engineered with modifications that enable them to better engage with immune cells.1 For example, the antibody obinutuzumab was engineered with modified sugars on the fragment crystallisable (Fc) portion of the antibody, providing greater potential to induce anti-tumour efficacy. A new therapeutic antibody class, bispecific antibodies, was engineered to build on the classic antibody design and bind to two different proteins, demonstrating how incremental changes in protein design can lead to entirely new therapies.2
Another immunotherapy treatment option, CAR T-cell therapy, involves collecting a patient’s T cells and engineering them to produce surface proteins known as chimeric antigen receptors (CARs).3 The CARs recognise and bind to proteins on the surface of cancer cells, effectively killing them. CAR T-cell therapies have been approved to treat multiple cancer types, including blood cancers such as lymphomas, multiple myeloma and some leukaemias. However, to date its application for solid tumours has been challenging. Additionally, CAR T-cell therapies must be customised for each patient, potentially making therapy access challenging. To address this, several companies are investigating advanced biomedical engineering techniques, such as CRISPR, to generate novel CAR T-cell therapies with shorter wait times.4
Harnessing the power of cytokines
Cytokines are immune-signalling proteins that have long shown promise as a therapeutic option for many diseases including cancer. A synthetic version of the cytokine interleukin-2, or IL-2, known for its potent effects on immune cells, was approved to treat metastatic melanoma and kidney cancer more than 20 years ago – making it the first approved immuno‑oncology treatment. Although IL-2 was recognised as an efficacious treatment, clinical use was limited by toxicity issues. IL-2 therapy is associated with safety concerns, namely the adverse event capillary leak syndrome, which often leads to hospitalisations and thus limits its clinical use. In addition, high doses of native IL-2 can activate suppressive immune cells that counteract the anti‑tumour effects of CD8 T cells and NK cells.5
With the advent of new protein engineering capabilities and the increasing understanding of the immune system, researchers are now able to design cytokines intended to mitigate some of these issues. The field of IL‑2‑based immunotherapy is an example of such novel design approaches.
Engaging the innate immune system to fight cancer effectively
Challenges of protein engineering
Several companies have focused on developing investigational IL-2 therapies, utilising advanced technologies to re‑engineer the IL-2 protein to retain its anti-tumour effects while minimising safety concerns. Protein engineering comes with several challenges, including maintaining stability and immunogenicity of the novel protein and creating an inherently active drug. Some approaches have relied on introducing chemical entities to the IL-2 protein, with the goal to direct its activity only towards cancer‑fighting immune cells. Others have modified IL-2 to be administered as a prodrug that is activated inside the body via metabolic cleavage. While these approaches have validated the potential of IL-2 as an immunotherapy, full clinical development has been hindered by suboptimal data in clinical trials, further underscoring the challenges of effectively re-engineering this molecule.
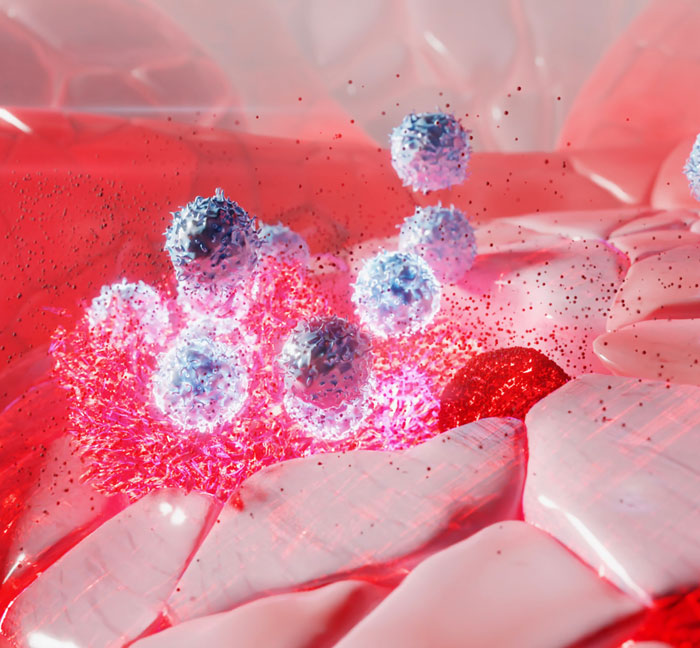
Immunotherapies help the immune system recognise and attack cancer cells.
Additionally, clinical trials of novel immunotherapies, including IL-2–based therapies, are often designed using combinations with immune checkpoint blockade, making it difficult to isolate monotherapy activity of the investigational agent. Establishment of single-agent activity is a critical component to consider in the development of new drugs, as eliciting the component effect of each molecule (in a combination) is critical in clinical development and, ultimately, regulatory approval.
At Alkermes, we have taken a unique approach to redesigning IL‑2. Our investigational IL-2 therapy nemvaleukin alfa (nemvaleukin), is an engineered fusion protein developed by fusing a modified IL-2 protein with a subunit of its own receptor, the high‑affinity IL-2 receptor alpha chain.6 This molecule was designed with the goal of retaining anti-tumour activity of IL-2 and preferentially expanding anti‑tumour immune cells (T cells and NK cells) while mitigating potential drawbacks of high-dose native IL-2 that lead to immunosuppression and toxicity. The molecule is a stable fusion protein that is administered as an active drug and does not degrade into native IL-2 inside the body. Early clinical trials have demonstrated clinical activity of nemvaleukin in patients pretreated with CPIs, as monotherapy, and in combination with pembrolizumab in tumour types, including those that are approved and unapproved for pembrolizumab treatment.
Protein engineering comes with several challenges, including maintaining stability and immunogenicity of the novel protein and creating an inherently active drug
In these early studies, particularly encouraging results were seen in mucosal melanoma and platinum-resistant ovarian cancer (PROC), which are both difficult-to-treat tumour types. Data from these early studies have paved the way for ongoing, later-phase clinical trials in mucosal melanoma and PROC. Nemvaleukin is being investigated as a monotherapy for patients with mucosal melanoma who progressed on immune CPIs, and for PROC as monotherapy and in combination with pembrolizumab. Nemvaleukin received several regulatory designations for development programmes from the US Food and Drug Administration (FDA) in 2021: Orphan Drug Designation and Fast Track Designation for mucosal melanoma and Fast Track Designation for the treatment of PROC. Additionally, nemvaleukin received entry into the Innovative Licensing and Access Pathway (ILAP) in the UK earlier this year for the treatment of mucosal melanoma.
Re-engineered immunotherapies: a turning point for immuno-oncology
Re-engineered immunotherapies have the potential to provide new treatment options in oncology that may help expand the range of cancers and the patient population that can be treated with these therapies. As continued research deepens our understanding of protein engineering and the immune system, we will continue to work relentlessly to develop new treatment options for oncology patients with difficult-to-treat tumour types.
About the author
Jessicca Rege, PhD serves as Vice President, Clinical Research Oncology at Alkermes, where she is responsible for establishing the company’s immuno-oncology development strategy and overseeing the execution of its global clinical trials. Dr Rege joined Alkermes in 2020, bringing with her more than 15 years of experience in research, clinical development and global medical affairs. She previously held roles of increasing responsibility at Bristol-Myers Squibb, Eisai, Daichi Sankyo and Boehringer Ingelheim. Dr Rege earned a Bachelor of Science from Carson-Newman, and holds both a Master of Science in Physiology and a PhD in Pharmaceutical Sciences from Virginia Commonwealth University. She completed her postdoctoral fellowship in paediatric leukemia at the University of Pennsylvania’s Children’s Hospital of Philadelphia.
References
- Alduaij W, Illidge T. The future of anti-CD20 monoclonal antibodies: Are we making progress? Blood. 2011; 117(11): 2993–3001.
- Salvaris R, Ong J, Gregory GP. Bispecific antibodies: A review of development, clinical efficacy and toxicity in B-cell lymphomas. J. Pers. Med. 2021; 11(5): 355.
- Alnefaie A, Albogami S, Asiri Y, et al. Chimeric antigen receptor T-cells: An overview of concepts, applications, limitations, and proposed solutions. Front. Bioeng. Biotechnol. 2022; 10.
- Dimitri A, Herbst F, Fraietta J. Engineering the next-generation of car T-cells with CRISPR-Cas9 gene editing. Mol Cancer. 2022; 21(1).
- Tang A, Harding F. The challenges and molecular approaches surrounding interleukin-2-based therapeutics in cancer. Cytokine: X. 2019; 1(1): 100001.
- Lopes J, Fisher J, Flick H, et al. Alks 4230: A novel engineered IL-2 fusion protein with an improved cellular selectivity profile for cancer immunotherapy. J Immunother Cancer. 2020; 8(1).
The post Re-engineering proteins to develop novel immunotherapies appeared first on European Pharmaceutical Review.

